We don’t yet have true PREVENTION of breast cancer through diet, and it’s misleading to use that term as if we do. We can certainly adopt preventive lifestyle strategies and habits, but for now, the most accurate and truthful term is “risk reduction.”
As of this writing, there are 167.5 million women in the United States. Approximately 6,000 U.S. women reach menopause every day. (1, 2)
Major diseases that impact postmenopausal women; heart disease, breast and colorectal cancer, and osteoporotic fractures, require targeted strategies in both prevention and treatment. The approaches health care providers take to diagnose, treat and educate on these disease states has come a long way, thanks in part to the Women’s Health Initiative.

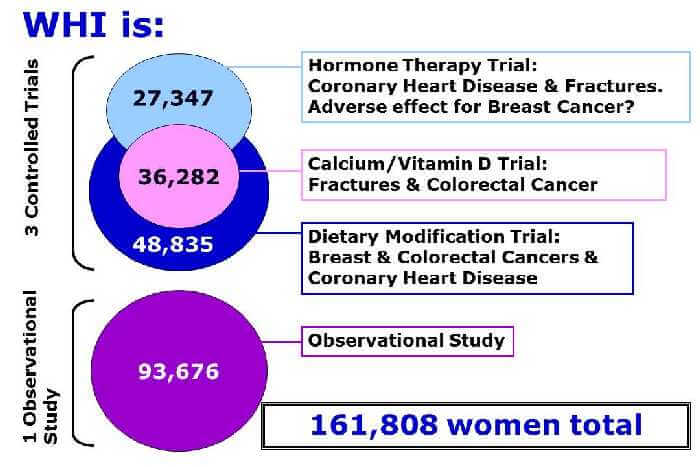
The Women’s Health Initiative is a multi-million dollar, 20+ year national health study focusing on the prevention of heart disease, breast and colorectal cancer, and osteoporotic fractures in postmenopausal women. In older women, regardless of race and socioeconomic background, these chronic diseases are the major causes of death, disability and frailty. (3)
This robust study was one of the most definitive, far-reaching clinical trials of postmenopausal women’s health ever undertaken in the U.S., and will continue into the future to provide practical information to inform women and their physicians.
The Observational Study portion continues to examine the relationship between lifestyle, health and risk factors and specific disease outcomes, and involves tracking the medical history and health habits of 93,676 women.
Each aspect of the study (hormone therapy trial, calcium/vitamin D trial and dietary modification trial) aids the effort to improve women’s health, yet as you may have guessed, I’m most interested in the Dietary Modification component, an evaluation of the effect of diet, specifically a low-fat, high fruit, vegetable and grain diet, on the prevention of breast and colorectal cancers and coronary heart disease.
Three dietitians heavily involved in the WHI research, Dr. Marian Neuhouser and Dr. Lesley Tinker from Fred Hutchinson Cancer Cancer Research Center in Seattle, WA (the WHI Clinical Coordinating Center for data collection, management, and analysis), and Dr. Linda Van Horn from Northwestern University Feinberg School of Medicine in Chicago, IL presented on the WHI study at a 2017 conference I attended; I share the information here.
Because this research continues to evolve and yield new findings, it was no small undertaking to distill volumes of information into an insightful overview and actionable directives we can use now, but the speakers succinctly shared the following take-home messages.
Insight Into Why SPECIFIC Breast Cancer Diet Protocols Don’t Yet Exist
Cancer cells are wily; able to successfully evade our immune system’s efforts to destroy them, replicate themselves many times over, invade and metastasize to other areas of the body, build new blood supply’s, and resist cell death.
Determining the EXACT way that food, dietary patterns and nutrition can outsmart and confer protection against a cancer cell’s innate arsenal remains elusive – yet researchers are making progress.

Nutrition, Diet and Its Impact on Cancer Initiation
We don’t yet have true PREVENTION of breast cancer through diet, and it’s misleading to use that term as if we do. We can certainly adopt preventive lifestyle strategies and habits, but for now, the most accurate and truthful term is “risk reduction.”
Still, findings exist that link diet and nutrition to a positive impact on the cancer disease process at several points, specifically: DNA repair, cellular proliferation, differentiation, the cell cycle and apoptosis (cell death).
How does diet do that?
Per Dr. Neuhouser, “These mechanisms are influenced by nutrients – primarily micronutrients – that act as co-factors of enzymes that up-regulate or down-regulate these pathways. Energy intake also plays a role, because macronutrient intake leads to insulin secretion, and hyper insulin secretion up-regulates the cell proliferation pathways.”
What this means in lay person’s language. . .
Micronutrients are nutrients in food that the body needs in small amounts; vitamins and minerals.
Macronutrients are foods required in large amounts; carbohydrate, protein, fat (and water and fiber.)
Micronutrients (i.e. vitamins E, C, D, A and minerals like calcium, potassium and phosphorus) act like “helpers” (co-factors) to make other processes happen in the body, and macronutrients supply calories (making up our “energy intake”) to fuel the body.
It’s the action of these micro and macronutrients – too much or too little of either – in “regulating” certain pathways that help tame or spur on cancer cells in their proliferation or differentiation, support cells in their repair efforts, or encourage cell death.
The ability to one day know for certain which specific foods turn cancer cells on or off, how much to eat for targeted results, optimal meal timing guidelines, and micro and macronutrient distribution for each individual’s specific breast cancer is an exciting possibility.
This type of personalized nutrition protocol would make a significant impact on healing, treatment outcomes, risk reduction and PREVENTION.
What We Know FOR SURE
- Being overweight or obese is linked to nearly every common cancer in both men AND women.
- Lifestyle factors, exercise AND diet are responsible for ~30% of all cancers.
- A better diet is associated with lower risk of cancer deaths, which held true for all women in this study EXCEPT for those who started with a body mass index (BMI) >30.
- There appears to be an interrelationship between pre-diabetes and diabetes as risk factors for breast cancer, with obesity a contender as the link.
- We may see some differences in outcomes between the many different types of breast cancer and diet.
- Women who ate a high-fat diet at the start of the study (fat was reduced during the study through intervention) showed greater reduction in breast cancer risk (possibly connected to weight loss.)
- Over the long term, postmenopausal women who followed a diet consistent with the American Cancer Society guidelines on nutrition and other healthy diet indicators (i.e. American Institute for Cancer Research) had significantly lower breast cancer risk and mortality.
- Breast cancer takes years to develop; a healthy diet should be maintained long-term for the maximum health benefit.
Putting It Into PRACTICE
As I see it, the challenge for most women to effectively and consistently use the ACS nutrition guidelines lies in being told only WHAT to do, yet not instructed on HOW to implement and maintain these guidelines in real life, for life.
Below, in bold, you’ll find the “what-to-do.” I’ve added “how-to-do” bullet points to help you implement the “what”:
6 American Cancer Society Guidelines on Nutrition
- Eat a healthy diet, with an emphasis on plant foods.
- ⅔ of plate filled with vegetables.
- Eat a vegetable and/or fruit with each meal/snack.
- Choose foods and drinks in amounts that help you get to and maintain a healthy weight.
- Serve meals on small plates. Have seconds if you’re still hungry (are you REALLY?), yet refill plate only 50%.
- Take ⅔ of restaurant meals home as leftovers.
- Order smallest size available for beverages containing calories.
- Limit how much processed meat and red meat you eat.
- ≤ 18 ounces/week.
- Eat at least 2 1/2 cups of vegetables and fruits each day.
- Not sure how much that is? Use measuring cups to train your eye, or visualize 2 ½ fists full.
- Choose whole grains instead of refined grain products.
- Whole wheat pasta and flour.
- Brown rice.
- Quinoa, amaranth, whole grain (vs. pearled) barley, millet.
- If you drink alcohol, limit your intake.
- No more than 1 standard drink (defined below) per day for women or 2 per day for men:
- 12 ounces of regular beer
- 5 ounces of wine
- 1.5 ounces of distilled spirits
- A standard drink contains 14 grams of PURE alcohol (the true culprit behind the cancer connection, which has nothing to do with the VOLUME in your glass.) (4)
- For breast cancer, there is NO safe limit for alcohol.
- No more than 1 standard drink (defined below) per day for women or 2 per day for men:
I’m curious. Since your diagnosis, what changes (if any) have you made to your diet? Tell me in the comments!
_______________________________________
Thanks for reading my blog post!
I help post-treatment survivors of hormone-positive breast cancer end food fear, confusion and overwhelm, eat without stress and guilt, and rebuild their health so they can do the things they enjoy with the people they love.
I’m a registered dietitian, personal trainer, nutrition therapist and coach, speaker, and survivor of hormone-positive breast cancer.
Ready for professional support to rebuild your health and gain peace of mind?
Click this link and watch my HEALTH REBUILD video!
Get my FREE Lifestyle Choices Matter! Get Started Guide here
Follow me on Instagram @hormone.breastcancer.dietitian
Sources


